.jpg)
Sleep apnea is a surprisingly common disorder, quietly affecting nearly one billion people worldwide. When left untreated, it can lead to a cascade of problems: chronic daytime fatigue, serious cardiovascular issues, a perpetually sour mood, and an overall diminished quality of life. Thankfully, we have two highly effective therapies—CPAP and BiPAP—that can dramatically improve sleep quality and, by extension, overall health for those struggling with sleep-disordered breathing.
If you've recently received a sleep apnea diagnosis or are finding it tough to get comfortable with your current therapy, you're probably asking yourself: BiPAP vs CPAP—what's the real difference, and more importantly, which one is the right fit for me?
This guide aims to demystify both machines, breaking down their key features, explaining how they work, and helping you figure out which option might better suit your specific needs.
Dr. Daniel Jin Blum, Sleep Expert, Clinical Psychologist, Research Assistant Professor of Psychology says this about choosing between CPAP and BiPAP:
“Choosing between BiPAP and CPAP depends on your specific breathing needs during sleep—while CPAP provides continuous pressure, BiPAP offers variable pressures to support more complex cases.”
Ultimately, there are different pros and cons to CPAP and BiPAP, which one should consider based on their own individual condition. Before we dive into the nitty-gritty comparison, it's helpful to understand the basic function and purpose of each of these remarkable machines.
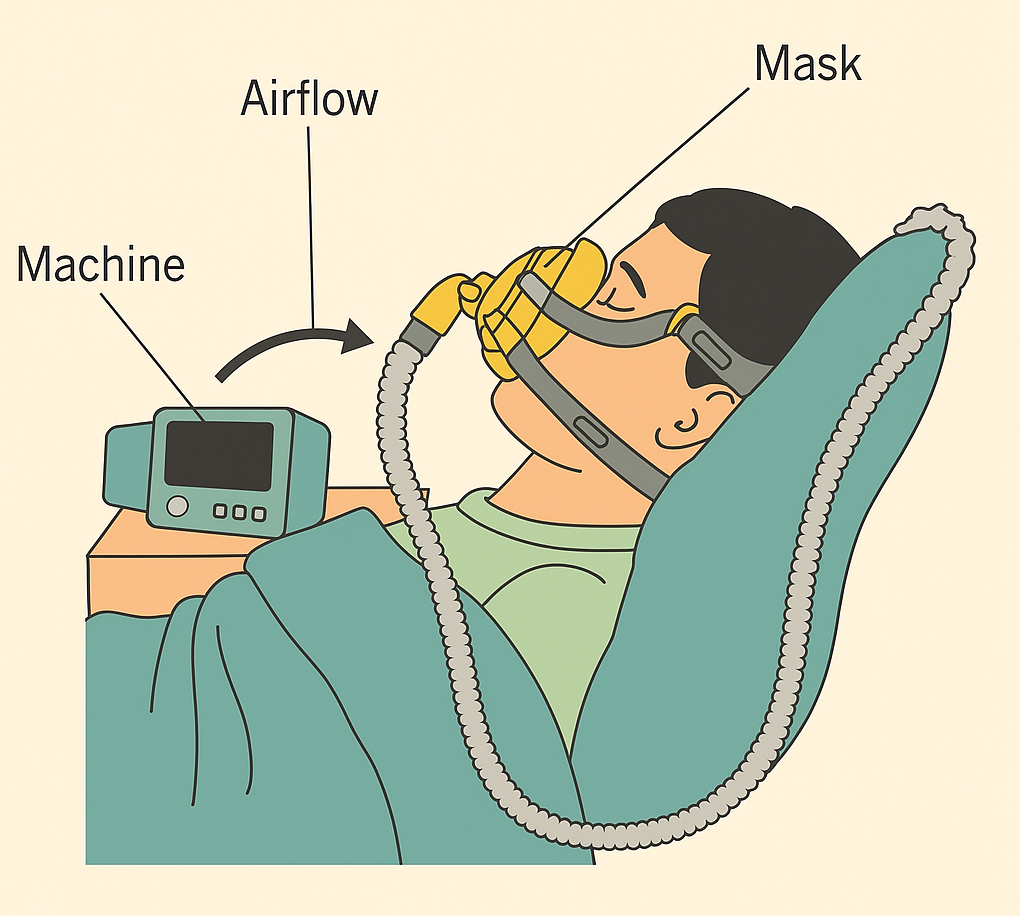
CPAP stands for Continuous Positive Airway Pressure. It's the most widely recognized and prescribed treatment for obstructive sleep apnea (OSA). The machine works by delivering a steady, constant stream of air pressure, maintaining an open airway throughout your sleep. This continuous positive airway pressure is crucial because it prevents the soft tissues in your throat from collapsing and causing those disruptive breathing interruptions.
Research demonstrates that CPAP therapy significantly reduces mortality and hospitalizations in patients with obstructive sleep apnea, with studies presented at the 2024 American Thoracic Society International Conference showing clear clinical benefits.
A typical CPAP setup usually includes:
BiPAP, short for Bilevel Positive Airway Pressure, also assists individuals with sleep apnea, but it does so with a clever twist: it uses two different air pressure levels or settings:
BiPAP machines are often recommended for more complex cases of sleep apnea or for individuals who simply can't tolerate the consistent pressure of standard CPAP therapy. Research has pointed to the effectiveness of BiPAP machines in improving gas exchange (oxygen levels for carbon dioxide) in patients with chronic obstructive pulmonary disorder (COPD).
While both machines share the fundamental goal of keeping your airway open during sleep, they diverge significantly in their functional approach, user comfort, and the specific conditions they're best suited for.
Many new CPAP users initially struggle with tolerance because exhaling against that fixed, continuous positive airway pressure can feel unnatural or even forceful. This is where BiPAP's dual-pressure system often shines. It can be significantly more comfortable, especially for those who require higher pressure settings to keep their airway open.
CPAP is almost always the first line of treatment recommended for obstructive sleep apnea. It's generally simpler to use, more budget-friendly, and incredibly effective when used consistently. The American Academy of Sleep Medicine's systematic review and meta-analysis found that the potential benefits of CPAP include reduction in OSA severity, improvement in patient symptoms (particularly sleepiness), sleep-related quality of life, and reduction in blood pressure.
Your sleep specialist will very likely suggest a CPAP if:
Despite its widespread use, some people do struggle with certain aspects of CPAP:
However, it's important to remember that many of these common issues can often be resolved with simple adjustments, such as adding a humidifier to the machine, trying a different face mask style, or utilizing pressure "ramp" settings that gradually increase pressure levels as you drift off to sleep.
BiPAP is generally prescribed when standard CPAP therapy isn't quite sufficient or proves to be intolerable. It's often the go-to for patients with:
Research on adaptive servo-ventilation therapy (a form of BiPAP) showed improved quality of life for central sleep apnea patients, particularly those on long-term opioid therapy.
It's also a considerably better fit for individuals who:
One of the most compelling reasons to treat sleep apnea with either CPAP or BiPAP is the potential cardiovascular protection. Sleep apnea causes episodic hypoxemia and nocturnal sympathetic nervous system activation, elevates blood pressure, and increases markers of oxidative stress, inflammation, and hypercoagulation.
Recent research has shown promising cardiovascular outcomes:
However, it's important to note that while observational studies show clear benefits, some randomized controlled trials have shown mixed results. The large SAVE trial found that CPAP therapy had no significant effect on preventing recurrent serious cardiovascular events in patients with established cardiovascular disease, though this may be due to factors like treatment adherence and patient selection.
We asked Dr. Shiyan Yeo, Internal Medicine Physician, Sleep Medicine Expert how to pick between the two options. She says:
“Proper titration and comfort with your device are key to treatment success, so working closely with your sleep specialist ensures the best fit for your sleep apnea therapy.”
In other words, it is important to choose wisely and make sure that you work with a professional to get the best fit. Choosing between CPAP and BiPAP isn't always a matter of personal preference. In many, if not most, cases, the results of your sleep study and your doctor's expert recommendations will directly dictate the most appropriate course of treatment. However, understanding how your comfort, lifestyle, and medical needs factor into the equation can empower you to advocate for the best possible solution.
If you're already using CPAP and struggling with discomfort or compliance, it's definitely worth having an open conversation with your sleep specialist about a trial with a BiPAP machine. Many users report immediate relief and significantly better adherence to therapy after making the switch. For those experiencing sleep maintenance insomnia or frequent nighttime awakenings, addressing sleep apnea with the right PAP therapy can be transformative.
The field of sleep apnea treatment continues to evolve rapidly. 2024 saw several significant advancements, including:
Research presented at major conferences continues to demonstrate that positive airway pressure therapy significantly reduces mortality and hospitalizations, reinforcing the importance of consistent treatment adherence.
Whether you end up using a CPAP or a BiPAP, your success with the therapy largely hinges on consistent adherence and ensuring maximum comfort. These tips apply equally to both types of airway pressure machines and can help you get the absolute most out of your treatment:
This is paramount for both comfort and effectiveness. Mask options abound:
Don't hesitate to try several types before committing to the one that truly feels best and provides a good seal.
Many modern CPAP and BiPAP machines come with built-in or attachable humidifiers. These are game-changers for combating common issues like dryness, nosebleeds, and uncomfortable mouth breathing.
Make it a habit to clean your face mask, hose, and water chamber at least once a week. This prevents the buildup of bacteria, mold, and allergens, keeping your therapy hygienic and effective.
Adjusting to sleep therapy takes time. It's common for people to feel a bit overwhelmed or give up too early. Try wearing the face mask during the day for short periods to simply get accustomed to the sensation.
Most contemporary airway pressure machines provide valuable compliance data and even basic sleep tracking. Use this feedback to troubleshoot any issues and, importantly, to stay motivated by seeing your improvements.
Choosing between CPAP and BiPAP is definitely not a one-size-fits-all decision. While CPAP remains an excellent first-line therapy for the majority of people with obstructive sleep apnea, BiPAP can be an absolute game-changer for those who require a more customized solution due to specific medical needs or intolerance.
The American College of Physicians recommends continuous positive airway pressure support as initial therapy for patients diagnosed with obstructive sleep apnea, but the evidence clearly shows that both CPAP and BiPAP can provide life-changing benefits when used consistently.
The most critical factor for success is consistent adherence to your therapy—whether that's with CPAP or BiPAP. Work closely with your doctor, respiratory therapist, or sleep specialist to fine-tune your settings, ensure you have the most comfortable equipment, and address any challenges that arise.
Getting the right airway pressure machine and using it consistently doesn't just promise better sleep; it's a vital investment in protecting your heart, brain, and long-term health. Research consistently shows that effective treatment of sleep apnea can significantly reduce cardiovascular risks and improve overall quality of life, making the effort to find the right therapy absolutely worthwhile.
Reach out to us at help@thesleepreset.com to learn more about CPAP and BiPAP therapy!
Take our Sleep Calculator and Chronotype Quiz to learn more about your sleep personality! If you're struggling with jet lag, try our Jet Lag Plan!

Dr. Areti Vassilopoulos | Psychologist | Sleep Medicine Expert
Dr. Vassilopoulos is the Clinical Content Lead for Sleep Reset and Assistant Professor at Yale School of Medicine. She has co-authored peer-reviewed research articles, provides expert consultation to national nonprofit organizations, and chairs clinical committees in pediatric health psychology for the American Psychological Association. She lives in New England with her partner and takes full advantage of the beautiful hiking trails.