This might have happened to you where the morning alarm goes off, and instead of the usual grogginess, you feel your heart racing at the thought of going to work. The average person probably feels some amount of dread when they think about going to work, much less someone who is already dealing with PTSD and anxiety. Another workday ahead and with it the challenge of navigating an environment that sometimes feels overwhelming when you're living with post-traumatic stress disorder (PTSD). If this sounds familiar, you're not alone and more importantly, there are effective strategies that can help you thrive professionally while managing your symptoms.
PTSD affects millions of people around the world - many developed after exposure to traumatic events ranging from accidents and natural disasters to assault or other life-threatening situations. 7-8% of Americans develop PTSD, though prevalence varies by population. This means actually almost 1 in every 10 people you meet experience PTSD in some shape. The global lifetime prevalence is 3.9%, with higher rates in certain populations.
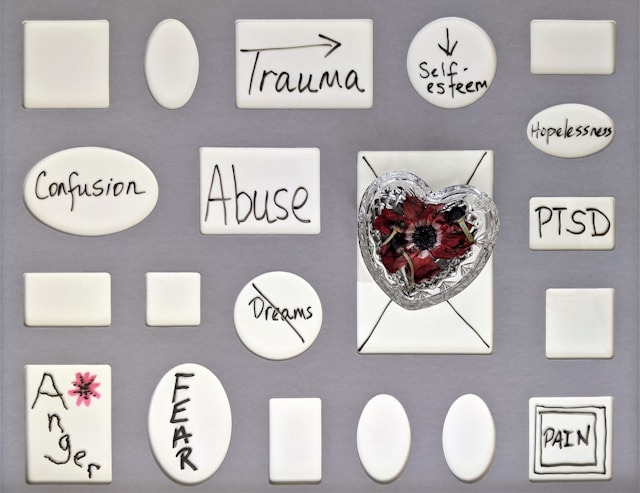
While the condition is commonly associated with military veterans, anyone can develop PTSD following trauma. Trauma is also such an all-encompassing word. You might ask what constitutes trauma? It could be a difficult experience you had with a coworker in the past, or a manager, or a client. In the workplace, symptoms like hypervigilance, difficulty concentrating, intrusive memories, or heightened stress responses can make daily tasks feel monumentally challenging.
The good news is with the right tools and support, you can successfully manage PTSD symptoms while maintaining a fulfilling career. Let us walk through some of these tools below.
Understanding your legal protections is very much empowering. ADA protects employees with PTSD, entitling you to reasonable workplace accommodations. PTSD qualifies as an ADA disability, and PTSD limits major life activities. These accommodations might include modified work schedules, the option to work remotely occasionally, a private workspace, or permission to take breaks when needed. You don't have to disclose specific details about your trauma, but communicating your needs to human resources or your supervisor can open doors to support.
Consider who in your professional circle can be part of your support system. This might include a trusted supervisor, HR representative, or colleague who understands your situation. Many people find that connecting with others who have similar experiences through support groups, either in-person or online, provides invaluable perspective and reduces feelings of isolation.
We asked Dr. Samantha Domingo, Sleep Expert and Clinical Health Psychologist, what her experience treating PTSD can tell us about work-related triggers. She says: “Creating predictable routines and safe boundaries at work helps individuals with PTSD reduce anxiety and maintain focus.” In other words, small environmental and structural adjustments can make a major difference in daily functioning.
Think of this as your personalized first-aid kit for difficult moments and your toolkit might include:
Grounding exercises for when you feel disconnected or overwhelmed. Grounding helps trauma survivors, reconnecting people to the present. The 5-4-3-2-1 technique works well: identify five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste.
Breathing techniques that activate your parasympathetic nervous system. Box breathing - inhaling for four counts, holding for four, exhaling for four, and holding for four—can be done discreetly at your desk. If you experience anxiety jolts when falling asleep, these calming techniques can help manage your body's fight-or-flight response at night. Many people with PTSD report adrenaline rushes during sleep, and understanding the causes and solutions can help you develop effective coping strategies.
Sensory anchors like a smooth stone in your pocket, a particular scent on a handkerchief, or a piece of familiar music on your phone that helps you feel grounded.
Planned breaks strategically placed throughout your day, even if just for five minutes, to reset and recharge.
Workplace triggers can be subtle: a particular sound, smell, anniversary date, or even certain conversation topics. Start keeping a simple log of moments when you notice symptoms intensifying. Over time, patterns will emerge. Once you identify triggers, you can develop specific strategies for each one. If crowded meetings trigger anxiety, perhaps you can position yourself near the door. If certain projects remind you of your trauma, discuss alternatives with your supervisor or first talk it over with HR or a more neutral party at the company.
Consistency can be remarkably stabilizing when living with PTSD. Establishing regular routines such as arriving at work at the same time, taking lunch breaks consistently, having an end-of-day ritual - creates a sense of predictability that can reduce anxiety. Similarly, setting clear boundaries about your workload and saying no when necessary protects your mental health.
A consistent sleep schedule is particularly important for managing PTSD symptoms. Try to wake up refreshed daily by maintaining regular sleep and wake times, even on weekends. If you find yourself constantly feeling tired despite getting adequate sleep hours, it may be worth exploring whether stress and PTSD symptoms are affecting your sleep quality over quantity.
Working with a mental health professional experienced in trauma isn't a sign of weakness, it's a strategic advantage. CBT and EMDR effectively treat PTSD. Both therapies are equally efficacious, with significant symptom reductions shown. EMDR matches other psychological treatments in effectiveness. A therapist can help you develop coping strategies tailored to your workplace challenges and provide ongoing support as situations evolve.
Many employers offer Employee Assistance Programs (EAPs) that provide confidential counseling services, often at no cost. These programs can be an excellent first step in accessing professional support.
If you're struggling with sleep issues related to PTSD and want to avoid medication, there are evidence-based natural sleep alternatives. Learning how to sleep without aids and exploring natural sleep remedies can be particularly helpful for those with PTSD who may be sensitive to medications or prefer non-pharmaceutical approaches.
Managing PTSD symptoms extends beyond the nine-to-five. Quality sleep, regular physical activity, nutritious meals, and stress-reduction practices like yoga or meditation all contribute to your resilience. When you're well-rested and physically healthy, you're better equipped to handle workplace stressors. For comprehensive guidance, explore these 15 tips for refreshing mornings and discover 11 ways to sleep better. You can also check out the ultimate guide to restful nights for evidence-based strategies.
Exercise enhances PTSD treatment, with physical activity reducing PTSD symptoms. More exercise provides greater benefits, and aerobic exercise reduces PTSD symptoms. Physical activity serves as adjunct therapy, with mental and physical health improvements.
Sleep disturbances commonly occur with PTSD, with 70-91% experiencing sleep difficulties. Sleep problems worsen PTSD course, and targeted sleep interventions reduce symptoms. Treating sleep aids PTSD recovery.
Improving your sleep quality at home is essential, and fortunately there are strategies for restorative sleep. If you're experiencing sleep anxiety or waking up at night, CBT-I transforms sleep. Learning how to break sleep anxiety and implementing improved sleep hygiene tips can make a significant difference in your recovery.
Getting adequate deep sleep and REM sleep is particularly important for emotional processing and trauma recovery. If you find yourself not feeling rested, this could be a sign that your sleep architecture is being disrupted by PTSD symptoms.
Don't underestimate the power of activities that bring you joy and connection, whether that's spending time with loved ones, engaging in creative pursuits, or connecting with nature. These aren't luxuries; they're essential components of your recovery and ongoing wellness.
Mindfulness reduces PTSD symptoms, with MBSR showing moderate effect sizes in clinical trials. All meditation types help PTSD, with significant PTSD severity reductions. Mindfulness increases trauma acceptance. If you're interested in learning more about the mind-body connection and CBT, these evidence-based approaches can complement your PTSD management strategy.
Sometimes despite our best efforts and accommodations, a particular work environment may not be conducive to managing PTSD symptoms. If you've implemented strategies, sought accommodations, and engaged in treatment but still find your workplace consistently triggering or unsupportive, it may be worth exploring other opportunities. Your health and well-being should always be the priority.
Living with PTSD while maintaining a career is undoubtedly challenging, but it's far from impossible. Thousands of people successfully navigate this reality every day, and with the right combination of self-awareness, professional support, workplace accommodations, and self-care strategies, you can too.
Remember that recovery isn't linear - there will be difficult days, and that's okay. What matters is that you have tools to manage those moments and the knowledge that support is available when you need it.
You deserve a workplace where you can contribute your talents while taking care of your mental health. By advocating for yourself, utilizing available resources, and maintaining your treatment plan, you're not just surviving, you're building a sustainable, meaningful professional life on your own terms.
If you're on medication or supplements and want to understand the potential side effects, read more about supplements like l-theanine or melatonin and what a melatonin hangover means as well as medication like ambien, dayvigo and quviviq. Or if you're ready to try Sleep Reset's unique CBT-I based program, take our free sleep assessment now to begin!
If you're struggling with PTSD symptoms, reaching out to a mental health professional is an important step. Many therapists specialize in trauma and can work with you to develop strategies specifically tailored to your workplace challenges. Don't hesitate to seek the support you deserve.

Dr. Areti Vassilopoulos | Psychologist | Sleep Medicine Expert
Dr. Vassilopoulos is the Clinical Content Lead for Sleep Reset and Assistant Professor at Yale School of Medicine. She has co-authored peer-reviewed research articles, provides expert consultation to national nonprofit organizations, and chairs clinical committees in pediatric health psychology for the American Psychological Association. She lives in New England with her partner and takes full advantage of the beautiful hiking trails.