.jpeg)
Not all sleep programs are created equal. Learn the key differences between therapy-style insomnia treatment and habit-based sleep systems — and which approach is right for your situation.
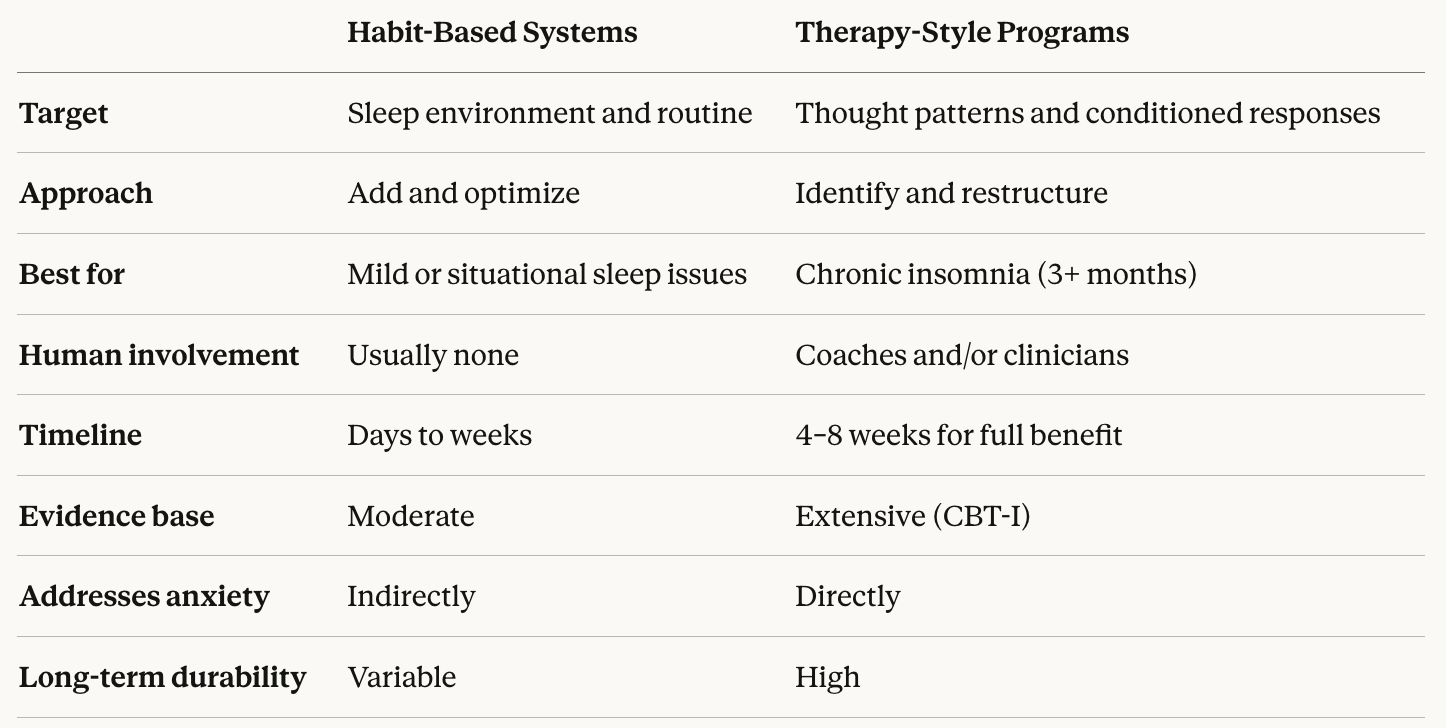
Walk into any conversation about sleep improvement and you'll encounter two fundamentally different schools of thought. One says: optimize your habits and environment, and sleep will follow. The other says: your insomnia is driven by learned patterns in your brain, and you need structured clinical treatment to undo them.
Both perspectives have merit — but they're suited to very different problems, and confusing the two is one of the main reasons people spend years trying things that don't work.
This guide breaks down exactly what separates therapy-style insomnia programs from habit-based sleep systems, helps you identify which approach fits your situation, and recommends the best therapy-style programs available right now.
Habit-based sleep systems operate on the premise that poor sleep is primarily a product of suboptimal conditions and routines. Fix the habits, the thinking goes, and the sleep will take care of itself.
These systems typically focus on:
This is broadly what's meant by sleep hygiene — and it's the foundation of most sleep apps, wellness blogs, and the advice your doctor probably gave you at your last check-up.
Habit-based systems genuinely help a significant number of people — specifically those whose sleep problems are mild, recent, or clearly linked to a specific lifestyle factor. If you started sleeping poorly after a stressful month at work, or you've been drinking coffee too late in the day, or your bedroom runs too warm, adjusting these factors can produce real improvement.
They're also a useful foundation for anyone going through a more structured treatment program. No therapy-style approach works in a vacuum — the behavioral conditions around sleep matter.
For anyone dealing with chronic insomnia — defined as difficulty sleeping at least three nights per week for three months or more — habit-based systems consistently underdeliver. Here's why:
Chronic insomnia is not primarily a habits problem. It's a learned problem. Over time, the brain becomes conditioned to associate the bed with wakefulness and anxiety. The arousal system becomes hyperactivated at night. Sleep anxiety develops and self-reinforces. Thoughts like "I'll never sleep normally again" or "I have to be asleep by 11 or tomorrow is ruined" create a performance pressure that no bedtime routine can dissolve.
No amount of lavender pillow spray or white noise changes those neural pathways. That requires therapy-style intervention — specifically, CBT-I.
Therapy-style insomnia programs are structured clinical interventions designed to identify and dismantle the psychological and behavioral mechanisms sustaining chronic insomnia. Rather than adding new habits to your routine, they systematically change how your brain and body relate to sleep.
The dominant framework — supported by decades of clinical research — is Cognitive Behavioral Therapy for Insomnia (CBT-I). It addresses insomnia at the level of thought patterns, conditioned responses, and sleep system dysregulation — the three layers that habit optimization simply can't reach.
Sleep Restriction TherapyThe most powerful and most misunderstood component of CBT-I. By temporarily limiting time in bed to match your actual sleep capacity, sleep restriction rapidly consolidates fragmented sleep and rebuilds sleep drive. It feels counterintuitive — and is temporarily uncomfortable — but the science behind sleep restriction therapy is among the most robust in sleep medicine.
Stimulus Control TherapyIf you've spent months lying awake in bed, your brain has learned that bed = wakefulness. Stimulus control systematically reverses this association, rebuilding the bed as a powerful sleep cue. This is the behavioral core of CBT-I and one of the reasons CBT-I produces results that outlast the treatment period.
Cognitive RestructuringSleep anxiety is sustained by a specific set of thought patterns — catastrophizing about consequences, unrealistic beliefs about sleep requirements, hypervigilance to bodily sensations at night. Cognitive restructuring directly addresses these patterns through structured therapeutic techniques. This is what separates CBT-I from relaxation approaches that merely try to calm anxious thoughts in the moment.
Sleep CompressionA gentler variant of sleep restriction particularly suited to older adults or people who can't tolerate abrupt changes. Sleep compression therapy gradually tightens the sleep window rather than imposing an immediate restriction.
Relaxation TechniquesBreathing exercises, progressive muscle relaxation, and mindfulness are used within CBT-I as supportive tools — not as the primary intervention. This is a crucial distinction: therapy-style programs use relaxation to reduce arousal, not to substitute for behavioral treatment.
The distinction isn't always obvious from the inside, so here are some reliable signals:
You probably need a habit-based approach if:
You probably need a therapy-style program if:
Not sure where you fall? Take the free insomnia assessment to get a clearer picture of your sleep health.
Sleep Reset is the most comprehensive therapy-style insomnia platform currently available online. It combines a proprietary CBT-I program with dedicated sleep coaching, licensed clinician oversight, and integrated medical services including home sleep testing for sleep apnea.
What sets it apart:
Every member is paired with a real sleep coach who personalizes their CBT-I program based on their specific insomnia pattern — whether the issue is falling asleep, staying asleep, or waking too early. The plan adapts week-to-week based on sleep diary data — making it one of the most personalized digital CBT-I programs available.
Sleep Reset also connects members with licensed sleep providers when medical evaluation is needed, and is covered by major insurance plans including Aetna, Blue Cross, and Anthem. HSA/FSA eligible.
Best for: Chronic insomnia of any duration; people who want human guidance; those on or looking to taper from sleep medication; anyone needing concurrent sleep apnea evaluation.
Read verified user reviews | See how Sleep Reset compares to competitors | Start with the sleep quiz
Working directly with a CBT-I trained therapist or sleep psychologist remains the clinical benchmark for therapy-style insomnia treatment. A therapist can offer the deepest level of personalization, handle complex presentations involving depression, PTSD, or anxiety disorders, and adapt in real time to your responses.
The limitation: Access is severely constrained. There are not enough CBT-I trained clinicians to meet demand, wait times can stretch to months, and sessions are expensive without robust insurance coverage. This is why more doctors don't routinely offer CBT-I and why digital platforms have become so important.
Best for: People with highly complex insomnia, co-occurring mental health conditions, or a strong preference for face-to-face care.
Sleepio is a digital CBT-I program developed by sleep researchers and validated in multiple clinical trials. It offers a structured, six-session self-guided program built around the core components of CBT-I, delivered through an automated online interface.
Strengths: Strong evidence base, widely used in research settings, available through some employer health plans.
Limitations: Fully self-guided — no human coach or clinician involvement. Adaptation is limited, which can be a challenge for people whose insomnia doesn't fit the standard profile. How does Sleep Reset compare to Sleepio? The primary difference is personalization and human support.
Best for: Motivated self-starters with straightforward insomnia who are comfortable working independently through a structured program.
Traditional sleep medicine clinics — whether in-person or via telehealth — offer the full spectrum of assessment and treatment, including polysomnography, home sleep testing, medication management, and CBT-I referrals. The benefits of telehealth for sleep issues have made this level of care considerably more accessible in recent years.
Limitations: Traditional clinics often focus on diagnosis and medication rather than behavioral treatment. CBT-I may be offered as a referral to a separate therapist rather than integrated into your care. Wait times for in-person appointments remain long in most areas.
Best for: People who need comprehensive diagnostic workup, have complex medical sleep disorders, or whose insomnia hasn't responded to behavioral treatment alone.
How is a therapy-style program different from everything else I've already tried?
Most sleep products work on the context of sleep rather than the cause of insomnia. What makes CBT-I genuinely different is that it targets the specific mechanisms — conditioned arousal, sleep anxiety, sleep system dysregulation — that sustain chronic insomnia regardless of how well everything else in your life is optimized.
I've had insomnia for over a decade. Is it too late for therapy-style treatment?
No. Even long-standing insomnia responds well to CBT-I. The learned patterns driving chronic insomnia can be unlearned at any age — the brain remains capable of change throughout life.
Will it work if my insomnia is caused by anxiety or depression?
CBT-I is effective even when insomnia co-occurs with anxiety or depression. In many cases, treating insomnia directly also improves mood and anxiety symptoms — the relationship between these conditions runs in both directions.
What if I'm currently taking sleeping pills?
CBT-I works alongside sleep medication and is the most evidence-backed path to safely tapering off prescription sleep aids long-term. A doctor-supervised taper combined with CBT-I is the clinical standard.
How long before I see results?
Most people notice meaningful improvement within 4–8 weeks of starting CBT-I. The first few weeks — particularly during sleep restriction — can be temporarily harder before sleep consolidates and improves significantly.
What if I'm not sleeping enough to even start a program?
CBT-I is safe even when you're running on very little sleep. In fact, sleep restriction works precisely because it starts from where you are — not where you want to be.
Habit-based sleep systems are a solid starting point — and a necessary foundation for any serious sleep improvement effort. But they were never designed to treat chronic insomnia, and they can't reach the cognitive and behavioral roots of a sleep system that has fundamentally gone off course.
If you've been doing everything "right" and still can't sleep, that's not a failure of discipline. It's a signal that you need a different level of intervention — one built around behavioral science, personalized to your specific insomnia pattern, and guided by real human expertise.
Take the free Sleep Reset quiz to find out where your insomnia comes from and which therapy-style approach is the right fit for you.
This article is for informational purposes only and is not a substitute for professional medical or psychological advice. Consult a qualified healthcare provider for diagnosis and treatment recommendations. See our editorial policy and medical expert team for more information.

Dr. Areti Vassilopoulos | Psychologist | Sleep Medicine Expert
Dr. Vassilopoulos is the Clinical Content Lead for Sleep Reset and Assistant Professor at Yale School of Medicine. She has co-authored peer-reviewed research articles, provides expert consultation to national nonprofit organizations, and chairs clinical committees in pediatric health psychology for the American Psychological Association. She lives in New England with her partner and takes full advantage of the beautiful hiking trails.