.jpeg)
If you've reached this conclusion, you're already ahead of most people still cycling through tip lists that go nowhere.
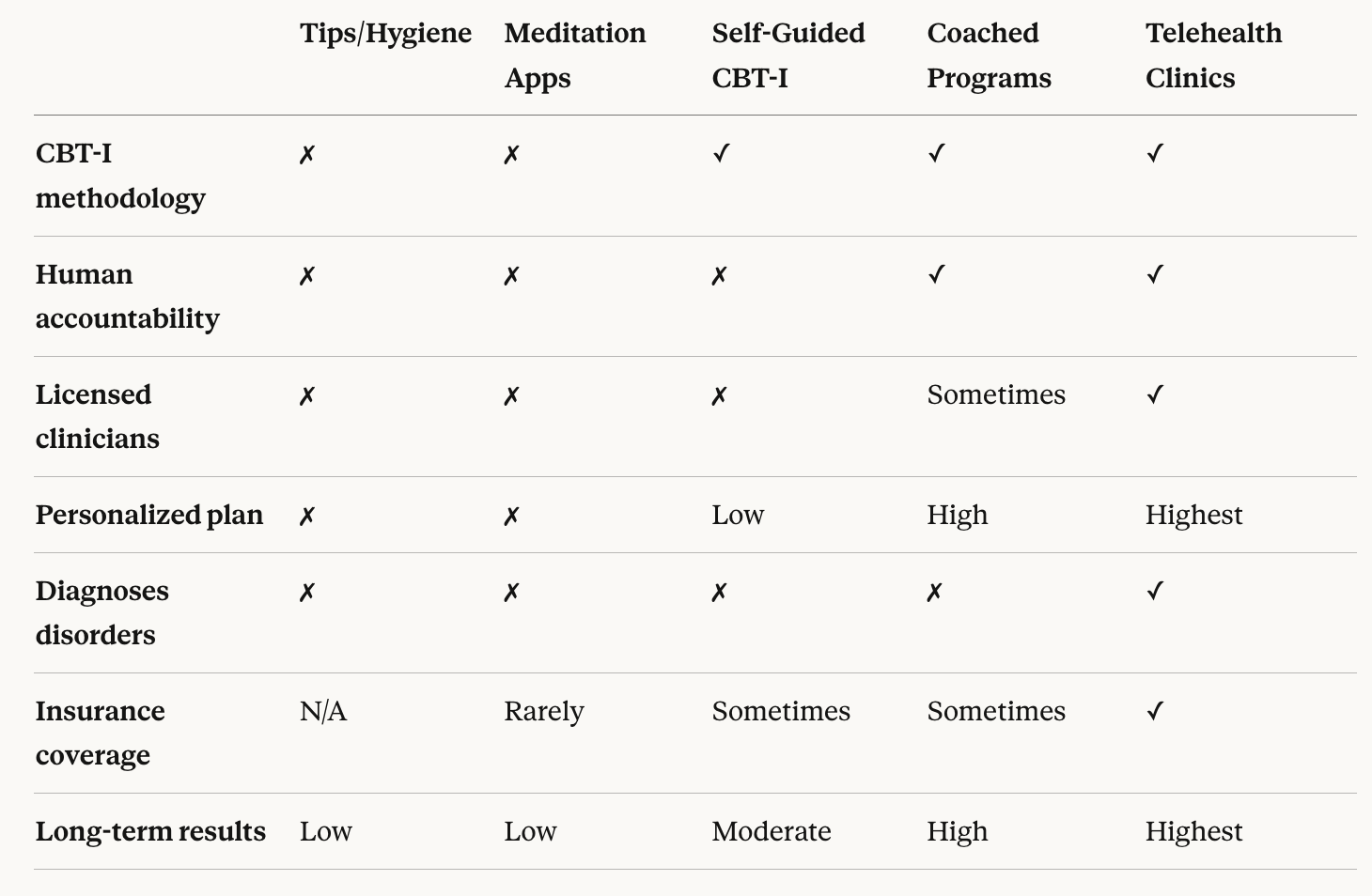
The realization that tips aren't enough — that what you actually need is a structured, systematic program — is the turning point most chronic insomnia sufferers reach after months or years of trying everything piecemeal. The next question is the right one: which programs are actually worth your time, and how do they compare?
This is an honest, side-by-side breakdown of the main sleep program categories — what each offers, what each lacks, and who each is right for.
Most people with chronic insomnia are not failing due to lack of effort. They're failing because they're using the wrong tool. A motivated person applying a self-guided meditation app to severe behavioral insomnia will get worse results than someone putting in half the effort with a properly structured, clinician-guided CBT-I program.
This matters because chronic insomnia is a conditioned behavioral and cognitive disorder. Your brain has learned — through hundreds of nights of lying awake — to associate bed with wakefulness, frustration, and anxiety. Reversing that conditioning requires a specific set of techniques applied in a specific sequence. Not every program does this. Most don't come close.
Before comparing programs, it helps to take a sleep quiz or insomnia test to understand what type and severity of sleep problem you're actually dealing with — because the right program depends heavily on that answer.
What they are: Articles, books, and content covering sleep hygiene practices — consistent schedules, evening routines, sleep environment optimization, caffeine limits, and so on.
What works: For people with mild, situational sleep difficulties, good sleep hygiene can produce real improvement. It's also a valid supporting layer for any program.
What doesn't work: For chronic insomnia, sleep hygiene alone consistently fails. It addresses surface behaviors but not the underlying behavioral conditioning and cognitive patterns that drive chronic sleep dysfunction.
Structure: None. Accountability: None. Personalization: None.
Best for: Mild, short-term sleep disruption. Not appropriate as a standalone treatment for chronic insomnia.
Cost: Free.
What they are: Apps like Calm, Headspace, and similar platforms offering guided meditation, breathing exercises, sleep stories, and relaxation content.
What works: These tools are genuinely effective at reducing pre-sleep arousal and nighttime anxiety. For people whose primary issue is racing thoughts at bedtime, they provide real relief.
What doesn't work: Relaxation is one component of good sleep — not a treatment for insomnia. These apps don't restructure the behavioral conditioning behind chronic insomnia, don't apply sleep restriction, and don't address the cognitive patterns that perpetuate it. Meditation-based apps are useful supplements, not standalone programs for chronic insomnia.
Structure: Moderate. Accountability: None. Personalization: Low.
Best for: Stress-related sleep disruption, relaxation support as part of a broader program.
Cost: $50–$100/year.
What they are: Digital platforms that deliver structured CBT-I content — sleep diaries, behavioral modules, sleep restriction protocols, stimulus control guidance — without any human involvement.
What works: The underlying methodology is sound. CBT-I is the gold-standard, first-line treatment for chronic insomnia — endorsed above sleeping pills by the American College of Physicians. For motivated users with straightforward insomnia, self-guided CBT-I can produce real results.
What doesn't work: Completion rates are notoriously low. Without accountability, most people quit during sleep restriction — exactly when it starts working. Apps also can't catch when you're applying techniques incorrectly, can't adapt dynamically to your real progress, and can't detect whether an underlying sleep disorder is complicating the picture.
Structure: High. Accountability: None. Personalization: Low to moderate.
Best for: Moderately motivated individuals with straightforward insomnia and no suspected underlying conditions.
Cost: $100–$300/year. Some covered by insurance.
What they are: Structured programs combining CBT-I content with dedicated sleep coaches who review your progress, adjust your plan, and provide regular check-ins.
What works: This is where outcomes shift meaningfully. Dedicated personal sleep coaches play an indispensable role in digital CBT-I programs — providing accountability through the hardest phases, catching misapplied techniques, and adapting plans based on real data rather than assumptions. Coached programs significantly outperform self-guided apps for chronic insomnia.
What doesn't work: Quality varies enormously. Some programs use general wellness coaches rather than sleep-trained specialists — a meaningful difference in how precisely CBT-I is applied. Always verify that coaches have specific sleep medicine training, not just general health coaching credentials.
Structure: High. Accountability: High. Personalization: High.
Best for: Moderate to severe chronic insomnia, anyone who has failed self-guided approaches, people who need accountability to follow through.
Cost: $200–$500+ depending on program length and coaching intensity. Insurance coverage increasingly available.
What they are: Virtual clinics staffed by licensed sleep medicine specialists — physicians, sleep psychologists, and board-certified clinicians — who assess, diagnose, and treat sleep disorders remotely, typically combining CBT-I programs with coaching and medical oversight.
What works: Everything. This is the most comprehensive level of sleep care available outside of an in-person lab. Telehealth sleep clinics can administer FDA-cleared home sleep tests, diagnose conditions like sleep apnea and restless legs syndrome, deliver CBT-I under physician supervision, and manage medication — all without leaving your home. For anyone with complex or long-standing insomnia, this is the category that closes cases rather than managing symptoms indefinitely.
What doesn't work: Access and cost were historically barriers — but telehealth has dramatically changed this. Many telehealth sleep clinics now accept major insurance plans and can be accessed with no wait time compared to in-person sleep specialists.
Structure: Highest. Accountability: Highest. Personalization: Highest.
Best for: Chronic insomnia of any severity, suspected underlying sleep disorders, anyone who has failed lower-level interventions, people currently on sleep medication seeking a supervised path off.
Cost: Varies widely; often covered by insurance. HSA/FSA eligible in many cases.
Is CBT-I really that much better than sleeping pills?
Consistently, yes. CBT-I outperforms sleep medication on long-term outcomes, with no dependency, no withdrawal, and benefits that compound after treatment ends. For anyone wondering whether CBT-I is better than Ambien or trazodone specifically, the research consistently favors CBT-I for lasting resolution.
What if I've already tried a self-guided app and it didn't work?
That's not evidence CBT-I doesn't work for you — it's evidence that self-guided delivery doesn't. Human-guided CBT-I is fundamentally different in practice. If apps and melatonin haven't worked, a structured evidence-based program is the clear next step.
How long does a real program take to work?
CBT-I typically produces meaningful results within 6–8 weeks, with many people noticing improvement within the first two to three weeks. Unlike medication, benefits continue growing after the active program ends.
Can I do a program while taking sleep medication?
Yes. In fact, coached and clinician-led programs are especially well-suited to helping you safely taper off prescription sleep aids as your sleep improves — something no self-guided app can responsibly manage.
What if I'm not sure whether I have insomnia or something else?
This is exactly why telehealth sleep clinics exist. Conditions like sleep apnea, restless legs syndrome, and delayed sleep phase syndrome frequently present as insomnia and require different treatment entirely. A proper clinical assessment rules these out — or identifies them — before you spend months on the wrong program.
Based on every meaningful criterion — clinical foundation, personalization, human accountability, diagnostic capability, and outcomes — Sleep Reset is the most comprehensive sleep program available.
It sits squarely in the telehealth sleep clinic category, but integrates coaching depth that most clinical platforms lack. Here's specifically what that looks like:
Clinically validated CBT-I methodology. Sleep Reset's proprietary CBT-I program is built and overseen by board-certified sleep specialists — not adapted from generic wellness content.
Dedicated personal sleep coaches. Not a shared support inbox. A specific coach assigned to your case, proactively reviewing your sleep diary and adjusting your program week by week.
Licensed sleep medicine specialists. Including Dr. Michael Grandner, Dr. Daniel Jin Blum, Dr. Areti Vassilopoulos, and Dr. Shiyan Yeo providing clinical oversight that separates Sleep Reset from coached-only platforms.
Home sleep testing. Physician-reviewed sleep apnea testing done from your own bed — with clear follow-up care built into the pathway.
Proven results. Users gain an average of 85+ more minutes of deep sleep. Physicians actively recommend Sleep Reset to patients who need real behavioral treatment.
Insurance coverage. Covered by major health plans. See pricing and coverage options or explore HSA/FSA eligibility.
Read verified user reviews, see how Sleep Reset is covered by press, or compare Sleep Reset directly against competitors before deciding.
Not all sleep programs are equal — and the gap between a tip list and a properly structured, clinician-guided CBT-I program is not a small one. It's the difference between managing insomnia indefinitely and actually resolving it.
If you're ready to move past tips and find the right program for your specific situation, take Sleep Reset's sleep quiz to map your sleep patterns and see how a personalized program would approach what you're dealing with. If you want to understand the clinical picture first, take the insomnia test to gauge severity before committing to a path.
The right program exists. Now you know what to look for.
This article is for informational purposes only and does not constitute medical advice. Please review our editorial policy and terms of service for more information.

Dr. Areti Vassilopoulos | Psychologist | Sleep Medicine Expert
Dr. Vassilopoulos is the Clinical Content Lead for Sleep Reset and Assistant Professor at Yale School of Medicine. She has co-authored peer-reviewed research articles, provides expert consultation to national nonprofit organizations, and chairs clinical committees in pediatric health psychology for the American Psychological Association. She lives in New England with her partner and takes full advantage of the beautiful hiking trails.