.jpeg)
Short answer: yes, consistently and significantly. But the longer answer explains why — and that context changes what you should actually be looking for.
Sleep tracking apps have become enormously popular. Tens of millions of people use wearables and apps to monitor their sleep stages, track their sleep scores, and get nightly readouts of how they performed. And yet chronic insomnia rates haven't budged. That gap — between the explosion of sleep tracking technology and the persistent failure to actually fix sleep — tells you something important about what tracking alone can and can't do.
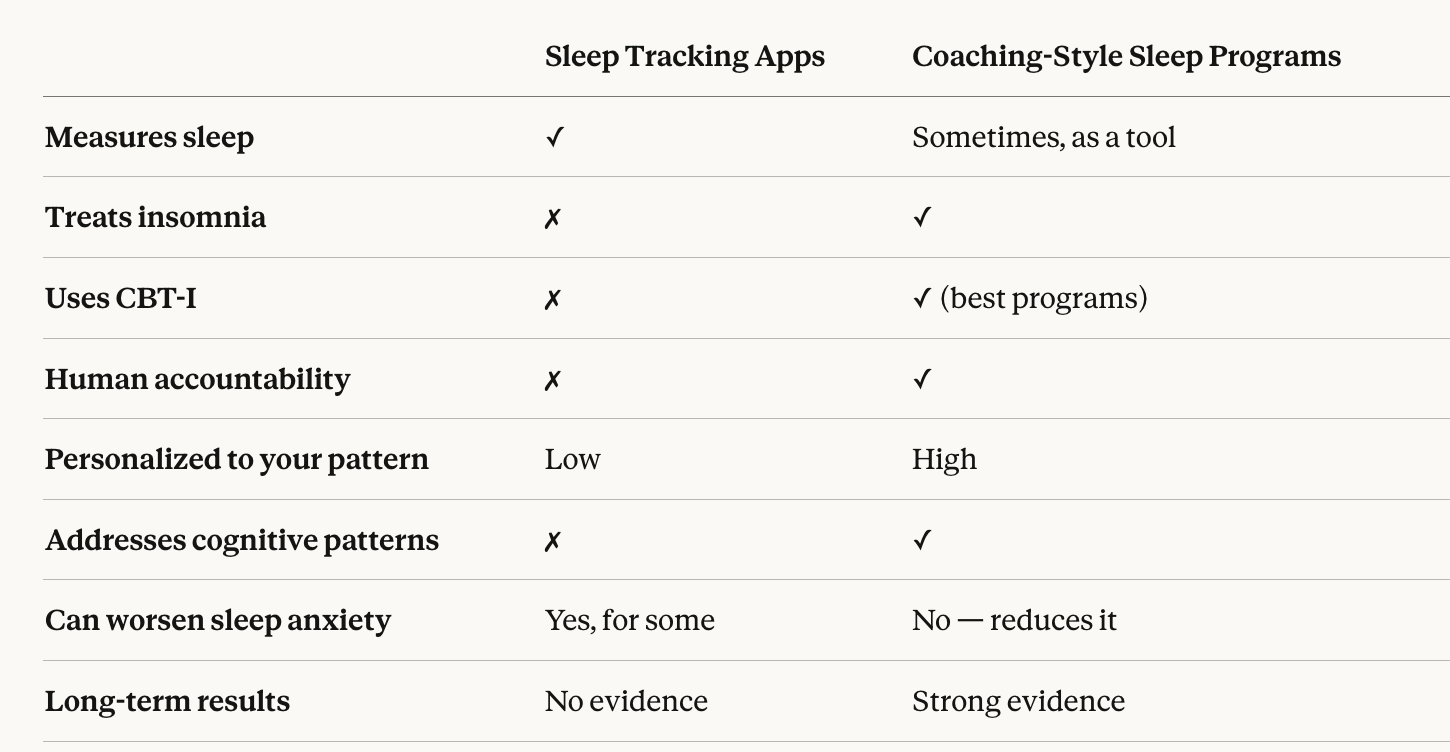
Coaching-style sleep programs operate on a fundamentally different premise: not monitoring your sleep, but changing it. Here's what the evidence says, how the two approaches compare, and which coaching-style programs are actually worth considering.
Sleep trackers — whether wearables like Fitbit, Oura, or Apple Watch, or app-based tools — measure proxies for sleep: movement, heart rate, heart rate variability, and sometimes blood oxygen levels. From these signals they infer sleep stages and generate a nightly sleep score.
This data can be genuinely interesting. But interesting is not the same as therapeutic. Here's where tracking falls short as a standalone approach to fixing sleep:
Tracking measures the symptom, not the cause. A sleep score tells you that you slept poorly. It doesn't tell you why — or what to change. For someone with chronic insomnia driven by conditioned behavioral patterns and cognitive hyperarousal, a nightly score is about as useful as a thermometer for someone with an infection. The measurement is accurate. The cure is elsewhere.
Tracking can actively worsen insomnia. For many people, obsessively checking sleep scores increases sleep performance anxiety — one of the primary cognitive drivers of chronic insomnia. There's a documented phenomenon sometimes called "orthosomnia" where people develop or worsen insomnia specifically from over-focusing on their tracked sleep data. Sleep anxiety and the pressure to perform are core contributors to chronic insomnia — and tracking often amplifies them.
Tracking doesn't intervene. Knowing you got 45 minutes of deep sleep last night doesn't rebuild your sleep drive, retrain your brain's bed association, or restructure the cognitive patterns keeping you awake. Sleep hygiene tips and tracking data are both passive — neither acts on the underlying mechanism.
Coaching-style sleep programs — particularly those built on CBT-I methodology — are active interventions. They don't measure your sleep. They change it. Here's specifically how:
The behavioral core of an effective coaching program involves two techniques that have no equivalent in tracking apps: sleep restriction therapy and stimulus control. Sleep restriction temporarily compresses your time in bed to consolidate your sleep drive and break the cycle of fragmented, inefficient sleep. Stimulus control systematically retrains the association between your bed and wakefulness that develops over months or years of lying awake at night. Both require precise implementation and human guidance to apply correctly.
CBT-I's cognitive component addresses the thought patterns that perpetuate insomnia: catastrophizing about bad nights, clock-watching, and the hypervigilance that turns every attempt to sleep into a test you can fail. This is the dimension of chronic insomnia that no tracker, app, or tip list ever touches — and the one that a trained sleep coach directly addresses through structured, personalized dialogue.
Dedicated personal sleep coaches play an indispensable role in CBT-I outcomes precisely because the most effective techniques are also the hardest to sustain without support. Sleep restriction involves feeling worse before feeling better — and this is where most self-guided attempts collapse. A coach who reviews your sleep diary, adjusts your program, and contextualizes your progress is the single biggest practical driver of whether CBT-I actually works.
A tracking app gives you the same interface regardless of whether you have sleep onset insomnia, sleep maintenance insomnia, or early morning waking. A coached program with a real clinician distinguishes between these presentations — and the treatment differs meaningfully depending on which pattern you have. Take a sleep quiz to identify your specific pattern before choosing a program.
Not all coaching programs are created equal. Here's an honest breakdown of the main options, what differentiates them, and who each is best suited for.
Sleep Reset is the most comprehensive coaching-style sleep program available — and the only one that fully integrates dedicated personal coaching, licensed sleep medicine clinicians, a proprietary CBT-I program, and home sleep testing in a single telehealth platform.
What sets it apart from every other coaching-style option:
Dedicated personal coaches — not a shared inbox, rotating staff, or automated chat. A specific sleep coach assigned to your case, proactively reviewing your sleep diary and adjusting your program weekly.
Licensed sleep medicine specialists including Dr. Michael Grandner, Dr. Daniel Jin Blum, Dr. Areti Vassilopoulos, Dr. Samantha Domingo, and Dr. Shiyan Yeo providing clinical oversight no coaching-only platform can match.
Diagnostic capability — if sleep apnea or another sleep disorder is underlying your insomnia, Sleep Reset identifies it through FDA-cleared home sleep testing rather than treating the wrong problem for months.
Proven, published outcomes — users gain an average of 85+ more minutes of deep sleep, and physicians actively recommend Sleep Reset to patients who need real behavioral treatment.
Insurance coverage through major health plans — see pricing and coverage or explore HSA/FSA eligibility.
Read verified user reviews, see independent press coverage, or compare Sleep Reset directly against competitors.
Best for: Anyone with chronic insomnia of any severity, people who have failed self-guided or app-based approaches, those on or trying to get off sleep medication, and anyone with suspected underlying sleep disorders.
Sleepio is a digital CBT-I program with a structured six-week course delivered by an animated character called "The Prof." It includes a sleep diary, weekly sessions, and automated progress tracking.
What works: The CBT-I content is solid and evidence-backed. For motivated users who complete the full program, results are meaningful.
What doesn't work: Sleepio is essentially self-guided — the "coach" is an algorithm, not a human. There's no dedicated specialist reviewing your data, no proactive adjustment of your plan, and no clinical oversight. For complex or long-standing insomnia, the absence of real human guidance is a significant limitation.
Best for: Mildly to moderately motivated individuals with straightforward insomnia who prefer a fully digital experience.
Somryst is an FDA-cleared prescription digital therapeutic delivering CBT-I over a nine-week program. It requires a prescription from a healthcare provider and is fully self-guided.
What works: FDA clearance provides a meaningful clinical validation of the CBT-I content. For people who can sustain a nine-week self-directed program, outcomes can be significant.
What doesn't work: Like other self-guided tools, completion and real-world effectiveness depend almost entirely on self-motivation. No human coach, no personalization beyond initial intake, and no diagnostic capability.
Best for: People with a healthcare provider willing to prescribe it and the self-direction to complete a nine-week solo program.
Traditional in-person CBT-I delivered by a licensed sleep psychologist remains clinically effective — and for some people, the preference for face-to-face care is meaningful.
What works: The gold-standard delivery of CBT-I with full human engagement and clinical expertise.
What doesn't work: Access is severely limited. Wait times for qualified CBT-I therapists often stretch months. Cost without insurance is high. Geographic availability is uneven. This is one of the primary reasons more people don't access CBT-I despite the evidence supporting it.
Best for: People with access to a qualified local CBT-I specialist and a preference for in-person care.
Can I use a tracking app alongside a coaching program?
Yes — as a supplementary data source, not a treatment. Sharing wearable data with your sleep coach can help them see patterns more clearly. What you want to avoid is letting the tracking become a source of sleep anxiety or replacing the structured behavioral work with passive monitoring.
I've tried self-guided CBT-I and it didn't work. Will a coached program be different?
Almost certainly yes. Self-guided and coached CBT-I produce meaningfully different outcomes even when the underlying techniques are identical. The methodology didn't fail — the delivery did. If apps and melatonin haven't worked, a human-guided program is the clear evidence-based next step.
How do I know if a coaching program is legitimate?
Look for programs with a clinically validated CBT-I methodology, coaches with verifiable sleep medicine training, published outcomes data, and real patient reviews. Be skeptical of programs that describe coaching but deliver it through automated messaging or general wellness coaches without specific sleep training.
Are these programs covered by insurance?
Increasingly yes. Telehealth sleep programs now qualify for coverage through major health plans including Aetna, Blue Cross, Anthem, and others. HSA and FSA funds are also eligible in most cases.
How quickly do coaching programs work compared to just using a tracker?
Most people following a coached CBT-I program see meaningful improvement within 2–4 weeks. Tracking apps produce no measurable improvement in insomnia outcomes on their own — by design, since they're measurement tools rather than treatments.
What if I have a condition like sleep apnea as well as insomnia?
This is exactly why clinical oversight matters. Sleep apnea frequently presents as insomnia and requires different treatment. A coaching program without diagnostic capability will treat the behavioral layer while missing the physiological driver entirely. Programs like Sleep Reset that include home sleep testing identify this before it becomes months of misdirected effort.
Sleep tracking apps and coaching-style sleep programs are not competing versions of the same thing — they're fundamentally different tools solving different problems. Tracking measures sleep. Coaching programs change it. For anyone dealing with chronic insomnia, the choice between them isn't really a choice at all.
The evidence for coached, CBT-I-based programs is unambiguous. They outperform apps, outperform meditation tools, outperform sleep hygiene tips, and outperform sleeping pills on long-term outcomes. Among coaching programs, the ones with real human coaches and licensed clinical oversight consistently produce better results than self-guided alternatives.
Take Sleep Reset's sleep quiz to map your specific sleep patterns and see what a personalized, coach-guided program would look like for your situation. Or take the insomnia test first if you want a clearer picture of what you're dealing with before taking the next step.
Your sleep score isn't the problem. Your sleep is. A coaching program is what actually fixes it.
This article is for informational purposes only and does not constitute medical advice. Please review our editorial policy and terms of service for more information.

Dr. Areti Vassilopoulos | Psychologist | Sleep Medicine Expert
Dr. Vassilopoulos is the Clinical Content Lead for Sleep Reset and Assistant Professor at Yale School of Medicine. She has co-authored peer-reviewed research articles, provides expert consultation to national nonprofit organizations, and chairs clinical committees in pediatric health psychology for the American Psychological Association. She lives in New England with her partner and takes full advantage of the beautiful hiking trails.